What You Should Know About SSI – Continuing Disability Reviews

Persons who have been awarded disability benefits, whether disability insurance benefits (SSD) or supplemental security income benefits (SSI) are subject to continuing disability reviews (CDR) regardless of age. The purpose of a CDR is to determine if one remains disabled. Generally, these reviews are conducted every three (3) years; however, SSA has wide latitude in determining when such reviews will be conducted.
The primary determinant of when a CDR is conducted depends on the nature of the medical condition that caused the disability and the permanency of that condition. Amputated arms and legs don’t grow back! Back pain can improve over time. Mental conditions may improve with psychotherapy and medications.
This article only addresses CDR’s based on whether your medical condition has improved enough to allow you to work. CDR’s may also be conducted when SSA determines that you have returned to work and are engaged in substantial gainful activity based on the level of your earnings or have exhausted your trial work period.
Continuing Disability Review Procedures

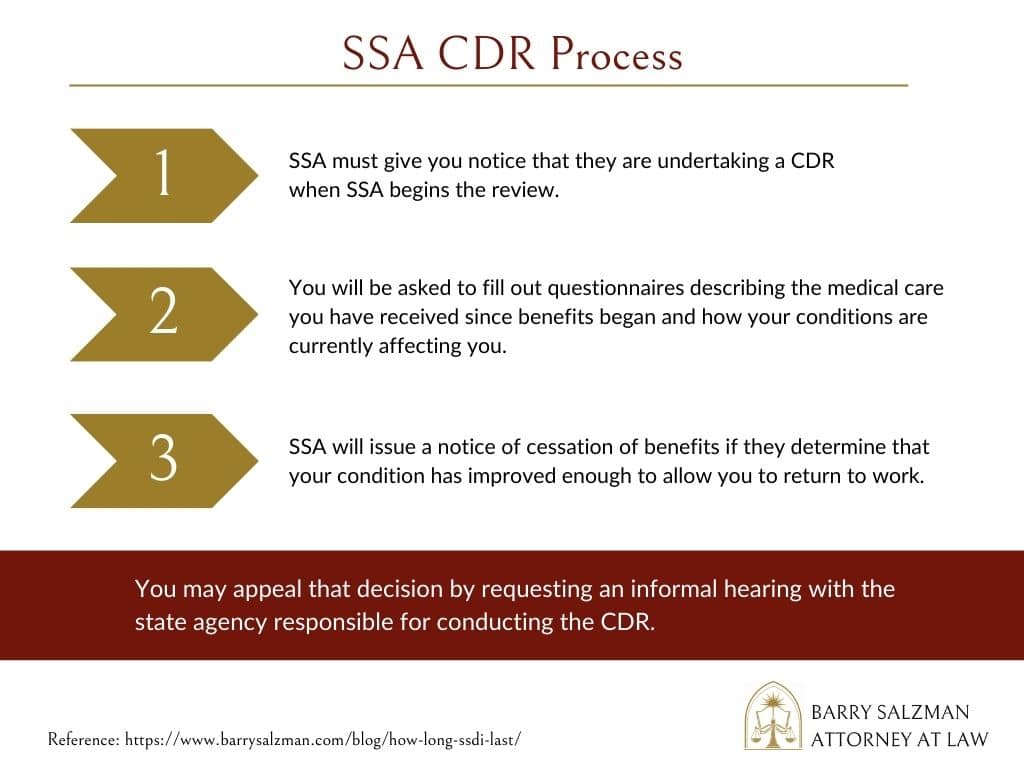
- SSA must notify you when they begin a CDR. You will be provided with questionnaires to complete, records of your medical treatment following the award of benefits will be acquired, and you may be referred for a medical or psychological examination.
- Your case will then be evaluated to determine if there has been improvement in your medical conditions sufficient to allow you to work. This evaluation also requires consideration of any new medical conditions that have arisen after you were awarded benefits. This evaluation will be conducted by the same state agency that initially evaluated your claim before you were awarded benefits.
- SSA will issue a Notice of Cessation if the state agency determines that your condition has improved sufficiently to allow you to work. If you disagree, you may appeal the decision within 60 days. You may also elect to have your benefits, including Medicare/Medicaid, continued while you appeal, provided you file your election within ten (10) days of the notice of cessation. Your appeal results in an informal hearing before a claims examiner with the state agency that made the decision to stop benefits.
- At the hearing, you will be able to testify, bring witnesses, and offer additional evidence to support your appeal. If your appeal is unsuccessful, a notice of reconsideration denying your appeal will be issued with a right to seek a hearing before an Administrative Law Judge for SSA within 60 days.
- As with your previous appeal, you may elect to continue your benefits while you await a hearing, provided you do so within ten (10) days of notice of the reconsideration.
- The Administrative Law Judge must make a new and independent determination of whether the medical condition for which you were awarded benefits has improved and is no longer disabling. If so, the judge must also consider whether you have any new conditions that are disabling. Of course, you have a right to present testimony at the hearing, present witnesses, and additional evidence. You may appeal an adverse decision to SSA’s Appeals Council.
What is “Medical Improvement”?
Medical Improvement (MI) is any decrease in the medical severity of an individual’s impairment(s) that was present at the time of the most recent favorable medical decision that the individual was disabled or continued to be disabled, known as the comparison point decision (CPD).
A finding of MI must be based on improvements in the symptoms, signs, or laboratory findings associated with the CPD impairment(s). Although the decrease in severity may be of any quantity or degree to find MI has occurred, minor changes in signs, symptoms, or laboratory findings are disregarded and do not represent MI and could not result in a finding that disability has ended.

Consider the following examples:
- At the CPD, an individual with a herniated nucleus pulposus underwent a laminectomy. A postoperative myelogram showed evidence of a persistent defect in the lumbar spine. The individual had pain in their back, as well as pain and a burning sensation in their right foot and leg. Evidence did not show muscle weakness or neurological changes, but it did show a moderate decrease in motion of the back and leg.
At the CDR, the evidence shows that the individual has received treatment from their primary care physician every two or three months for the past two (2) years. No further myelograms have been done. The individual continues to complain of pain in the back and right leg, especially when sitting or standing for more than a short period. The doctor reports a moderately decreased range of motion in the back and right leg and still reports no muscle atrophy or neurological changes.
Decision: No medical improvement. - At the CPD, benefits were awarded based on laboratory results showing inflammatory arthritis. The individual’s physician reported persistent swelling and tenderness of the individual’s fingers and wrists and noted that the individual complained of joint pain.
At the CDR, tests still show rheumatoid arthritis. However, because of therapy, the individual’s fingers and wrists have not been significantly swollen or painful for the past year. The decreased pain and swelling have led to an increase in the individual’s fine and gross manipulation. Changes in symptoms and signs show decreased medical severity.
Decision: Inflammatory arthritis is an example of an impairment subject to temporary remission, and the improvement demonstrated in this example has been sustained long enough to establish remission.
When are CDR’s conducted?
When benefits are awarded, each case is assigned a “medical review diary” based on the following categories:
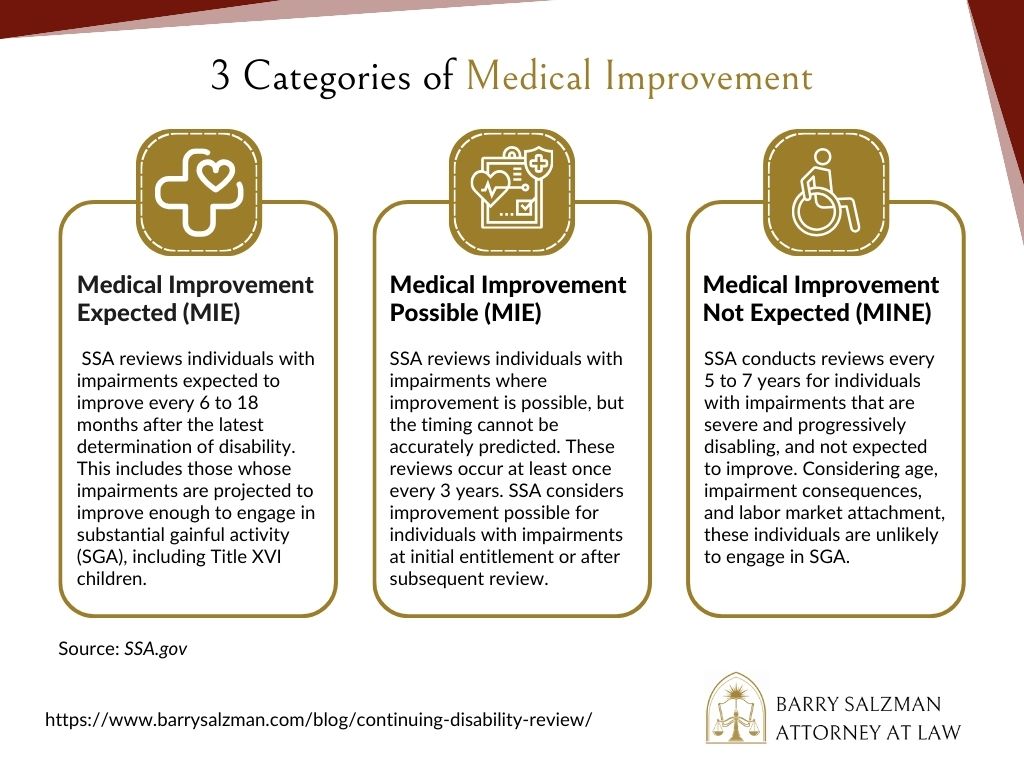
- Medical improvement expected: SSA will schedule a review of an individual with an impairment expected to improve at intervals from 6 to 18 months following the most recent determination or decision that the individual is disabled or that disability is continuing.
This review will apply to individuals with impairments, which, at the time of initial entitlement or after further review, are expected to improve sufficiently to permit the individuals to engage in substantial gainful activity (SGA). This review is also applicable to Title XVI children whose impairments expect to improve to the extent in which they no longer meet or equal a medical listing. - Medical improvement possible: SSA will schedule a review (at least once every three years) of an individual with an impairment in which any improvement is possible but which cannot be accurately predicted within a given period of time.
This review is applicable to individuals with impairments at the time of initial entitlement or after subsequent review in which SSA considers improvement possible. In these cases, improvement may occur to permit the individuals to return to SGA, but SSA cannot predict improvement with accuracy based on current experience and the facts of the particular case.
Such impairments are not at the level of severity of impairments in which improvement is not expected. - Medical improvement not expected: SSA schedules reviews of an individual with an impairment not expected to improve no less frequently than once every seven years but no more frequently than once every five years. These reviews apply to individuals with impairments at initial entitlement or after further review in which any improvement is not expected.
These are extremely severe impairments shown, on the basis of administrative experience, to be at least static but more likely to be progressively disabling of themselves or by reason of impairment complications. The individual is unlikely to engage in SGA.
We consider the interaction of the individual’s age, impairment consequences, and the lack of recent attachment to the labor market in determining whether impairment is expected to improve.
CDR may also be conducted when you have reported to SSA that your condition has improved and you have returned to work, when you have completed vocational rehabilitation services and the rehab agency reports that you are now able to work, or when someone in a position to know provides a credible report that you are no longer disabled or that you have returned to work or that you are not following prescribed treatment.
For example, your neighbor reports that you have been seen performing strenuous work activity around your house that is inconsistent with the allegations on which you were found disabled. Such reports usually result in an investigation by SSA’s Office of the Inspector General to determine if fraud has been involved.
Takeaways

- When SSA begins a CDR, they will first ask you to provide information about what medical care you have received since benefits were awarded. Often, claimants stop getting medical treatment when benefits are awarded.
- The absence of medical treatment may suggest that your condition is no longer as severe as you alleged when awarded benefits. Unless you have a static medical condition for which no medical treatment is available, continuation of medical care is essential.
- Regular medical care results in your doctor preparing office notes that chronicle your continuing symptoms and complaints. Those notes can provide sufficient evidence that no improvement has occurred.
- Not all efforts to return to work after an award of benefits will trigger a CDR; however, returning to even a part-time job that is beyond the functional limitations upon which you were awarded benefits can suggest medical improvement sufficient to allow you to return to work.
- CDR evaluations must consider age in the evaluation process. A CDR evaluation must be based on the same evaluation process required when benefits are awarded.
- If CDR occurs when you are under 50, SSA must only demonstrate that you can perform an unskilled job of a light or sedentary character.
- On the other hand, if you are age 55 or older when the CDR occurs, SSA must demonstrate that you are no longer able to perform the work you performed prior to your disability and that you are limited to no more than light or sedentary work and do not have transferable job skills that allow for direct entry into skilled light or sedentary work.
- If benefits were awarded due to chronic recurring conditions such as seizures, migraine headaches, or ulcerative colitis, you should keep a diary of how frequently these conditions cause disabling episodes and the severity of those episodes. That documentation provides very credible evidence of a continuing disability. In short, you must keep in mind that no award of disability benefits can be considered as “permanent”.
- All are subject to CDR. Act accordingly.
Need Help with Your Continuing Disability Review?
Never feel you’re alone in navigating the complexities of the Social Security Continuing Disability Review process. Whether you’re facing your first review or grappling with a negative determination, you need expert advice and support.
Don’t wait until you’re overwhelmed. Reach out to our team of experienced Social Security disability lawyer today. We’re here to help ensure your rights are protected, and you continue receiving the benefits you deserve. Remember, your future is too important to leave to chance. Contact Atty. Barry Salzman to schedule a free consultation.
Schedule Your Consultation Today
Navigating the bureaucracy of any disability program is complex and frustrating and often ends in denial.
Don't do it alone! Have a dedicated, experienced advocate on your team.
Fill out the form below or give us a call at 727-321-4993.